

How Ankylosing Spondylitis Affects More Than Just Your Spine
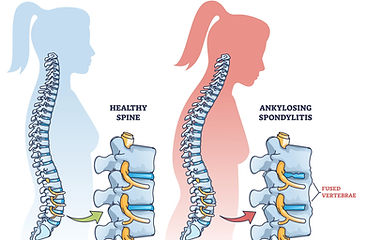
Ankylosing spondylitis (AS) is a chronic, inflammatory disease that primarily affects the spine and sacroiliac (SI) joints. It typically begins in early adulthood, often before the age of 40, and is marked by chronic back pain and progressive stiffness. Over time, the inflammation can lead to reduced spinal mobility, postural changes, and, in some cases, fusion of spinal joints.
While AS most commonly involves the axial skeleton, it is not limited to the spine alone. It can also affect peripheral joints, entheses (the sites where tendons and ligaments attach to bone), and digits.
Beyond the Joints: Extra-articular Manifestations
AS is more than just a spinal condition. It can affect other organs and systems, leading to:
-
Inflammatory bowel disease – occurs in up to 50% of individuals with AS
-
Acute anterior uveitis (eye inflammation) – seen in 25–35% of cases
-
Psoriasis – affects about 10% of patients
-
Cardiovascular disease – linked to systemic inflammation
-
Pulmonary complications – reduced chest expansion can lead to a restrictive breathing pattern
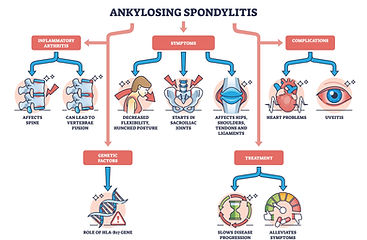
What Causes AS? The Role of Inflammation
The underlying pathology of AS involves enthesitis – chronic inflammation at tendon and ligament attachment sites. This process is driven by immune cells such as CD4 and CD8 T lymphocytes, as well as macrophages.
Inflammatory molecules, particularly tumour necrosis factor-α (TNF-α) and transforming growth factor-β (TGF-β), contribute to:
-
Ongoing inflammation
-
Fibrosis (scar tissue formation)
-
Ossification (abnormal new bone formation)
This immune-driven cycle is why AS is classified as a chronic autoimmune disease with strong genetic links. Recent research has identified several genes, such as ERAP1, TNFRSF1A, and IL12B, as potential therapeutic targets for the future.
Distinguishing AS from Other Conditions
Because chronic back pain is so common, AS can often be mistaken for other spinal conditions. Key differences include:
-
Mechanical back pain: Can occur at any age, improves with rest, and is not associated with systemic inflammation or extra skeletal features.
-
Lumbar spinal stenosis (LSS): Typically affects older adults (60+), may cause stiffness but lacks features like sacroiliitis or uveitis.
-
Rheumatoid arthritis (RA): More commonly involves peripheral joints and rheumatoid nodules, which are absent in AS.
-
Diffuse idiopathic skeletal hyperostosis (DISH): A degenerative condition with spinal ossification, but not an inflammatory disorder.
Kinesiophobia: The Fear of Movement
Many people with AS develop kinesiophobia, or fear of movement, due to pain and fear of injury. Unfortunately, this can limit physical activity and worsen stiffness. Research highlights that exercise therapy is one of the most effective strategies for managing AS, and overcoming movement-related fear is key to long-term function and quality of life.
Advances in Imaging and Research
Diagnosis and monitoring of AS have greatly improved thanks to imaging advances:
-
MRI: Highly sensitive for detecting early inflammatory changes in the sacroiliac joints.
-
Low-dose CT: Can identify structural changes like syndesmophytes with reduced radiation exposure.
On the research front, multi-omics studies have revealed promising genetic and molecular targets, paving the way for more effective treatments in the future.
Treatment: A Combined Approach
The goals of treatment are to:
-
Relieve pain and stiffness
-
Preserve spinal mobility and posture
-
Prevent long-term complications
Non-pharmacological management is essential and includes:
-
Exercise therapy
-
Postural training
-
Physiotherapy
Alongside this, non-steroidal anti-inflammatory drugs (NSAIDs) are typically the first-line pharmacological option. For those with more severe disease, targeted biologic therapies may be considered.
The Patient Perspective:
Recent studies have emphasized the importance of listening to patients’ experiences. Living with AS affects not only physical health but also emotional wellbeing, social participation, and quality of life. Understanding these perspectives helps healthcare providers offer more personalized care and improve outcomes.
Ankylosing spondylitis is a complex condition that goes beyond simple back pain. It involves the immune system, multiple body systems, and significantly impacts daily life. With the right combination of exercise, medical therapy, and patient-centred care, people with AS can maintain mobility and improve their quality of life.
References
-
StatPearls [Internet]. Ankylosing Spondylitis. NCBI Bookshelf.
-
PeerJ. Ankylosing spondylitis and kinesiophobia.
-
Progress in targeted therapy for ankylosing spondylitis: A review. PMC.
-
Experiences and perceptions of patients with ankylosing spondylitis: A systematic review and meta-synthesis of qualitative studies. PLOS One.
-
The history of ankylosing spondylitis/axial spondyloarthritis – what is the driving force of new knowledge? ScienceDirect.
-
Identifying prioritization of therapeutic targets for ankylosing spondylitis: A multi-omics Mendelian randomization study. PMC.

